GERD
- Home
- Service
GERD
GERD stands for gastroesophageal reflux disease. It is a chronic digestive disorder characterized by the frequent or persistent reflux of stomach acid and contents into the esophagus, causing a range of symptoms and potential complications.
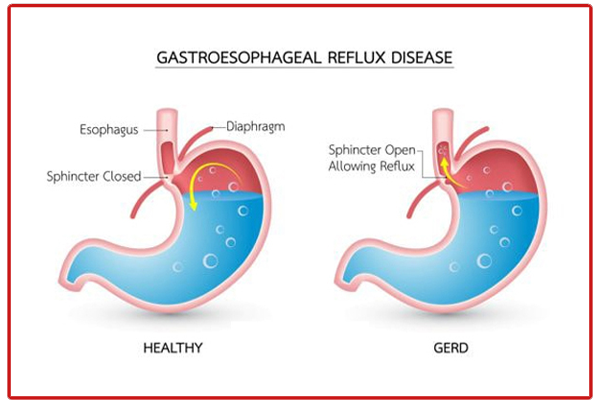
In a healthy digestive system, a muscular ring called the lower esophageal sphincter (LES) acts as a barrier between the stomach and the esophagus, preventing the backflow of stomach acid. However, in individuals with GERD, the LES may weaken or relax abnormally, allowing stomach acid and digestive juices to flow back into the esophagus.
Symptoms of GERD
Symptoms of GERD can vary in severity and frequency but commonly include:
Heartburn: A burning sensation or discomfort in the chest, often after eating or when lying down.
Acid Regurgitation: The perception of a sour or bitter taste in the mouth, caused by the backflow of stomach acid into the throat or mouth.
Difficulty Swallowing: Also known as dysphagia, this can occur when acid reflux causes irritation and narrowing of the esophagus.
Chest Pain: Chest pain may mimic the symptoms of a heart attack, although it is usually unrelated to the heart.
Chronic Cough and Hoarseness: Repeated coughing, hoarseness, or a sensation of a lump in the throat due to irritation from stomach acid reaching the throat.
Causes of GERD
Gastroesophageal reflux disease (GERD) can have multiple causes, and it often involves a combination of factors. Common causes and contributing factors include:
Weak Lower Esophageal Sphincter (LES)
Hiatal Hernia
Obesity
Pregnancy
Delayed Stomach Emptying (Gastroparesis)
Certain Foods and Beverages: Spicy foods, fatty or greasy foods, citrus fruits, tomatoes, chocolate, caffeine, alcohol, and carbonated beverages.
Smoking
Medications: Such as NSAIDs, calcium channel blockers, beta-blockers, sedatives, and some asthma medications.
Connective Tissue Disorders: Such as scleroderma.
It’s important to note that not everyone who experiences occasional acid reflux will develop GERD. However, if symptoms are persistent, frequent, or significantly impact daily life, it is recommended to seek medical evaluation.
Factors contributing to GERD include obesity, hiatal hernia, pregnancy, certain medications, smoking, and a diet high in fatty or spicy foods, caffeine, and acidic foods.
If left untreated, GERD can lead to complications such as:
Esophagitis (inflammation of the esophagus)
Esophageal strictures (narrowing of the esophagus)
Barrett’s esophagus (abnormal changes in the lining of the esophagus)
Increased risk of esophageal cancer
Treatment
Treatment options for GERD aim to alleviate symptoms, heal esophageal damage, and prevent complications:
Lifestyle Modifications: Weight loss, elevating the head of the bed, avoiding trigger foods, and quitting smoking.
Medications: Over-the-counter antacids or prescription medications like proton pump inhibitors (PPIs) to reduce stomach acid.
Surgery: In severe or unresponsive cases, procedures like fundoplication may be recommended to strengthen the LES and prevent reflux.
If you suspect GERD or experience persistent acid reflux symptoms, consult a healthcare professional for diagnosis and treatment.
Prevention
To help prevent GERD symptoms, try the following:
Maintain a Healthy Weight
Eat Smaller, More Frequent Meals
Avoid Trigger Foods and Beverages
Eat Mindfully: Chew food thoroughly and eat slowly.
Maintain Good Posture During and After Eating
Elevate the Head of Your Bed: 4–6 inches to prevent nighttime reflux.
Avoid Eating Before Bedtime: Allow 2–3 hours after eating before lying down.
Quit Smoking
Manage Stress
Avoid Tight-Fitting Clothing
These lifestyle modifications may not completely eliminate GERD symptoms for everyone. If symptoms persist, consult a healthcare provider. They may recommend medications or other interventions.
When to See a Doctor
GERD symptoms are treatable. Modifying your eating and sleeping patterns and using medications can help reduce symptoms. Contact your doctor if:
You have heartburn or acid reflux more than twice per week over several weeks
You frequently use antacids or heartburn medications
Your symptoms persist or worsen despite treatment
